Fungal Acne Vs Closed Comedones: Everything You Need To Know
This post may contain affiliate links.

What Is The Difference Between Closed Comedones And Fungal Acne
Believe it or not, there are many different types of acne – comedonal acne, inflammatory acne and fungal acne are just a few of the most common types. While some may look incredibly similar, their causes, symptoms and treatment are all very different. Fungal acne and closed comedones are two types of acne that often get confused because they can look so similar to each other. But they are incredibly different! In fact, fungal acne isn’t acne at all. So if you’re confused about the differences between fungal acne vs closed comedones, then keep on reading for everything you need to know including causes, symptoms, how to tell them apart and effective treatments.
What Is Fungal Acne
Contrary to what it sounds like, fungal acne isn’t actually acne at all. Regular acne is caused by a combination of factors such as oil production, bacteria and dead skin cells clogging pores. Fungal acne is caused by yeast called Malassezia yeast that’s naturally found on the skin and leads to an infection in the hair follicles.
Also known as pityrosporum folliculitis or malassezia folliculitis, fungal acne occurs when there’s an overgrowth of yeast which can lead to acne like breakouts.
Although fungal acne can differ in presentation, it usually closely resembles regular acne and can cause whiteheads, papules, pustules and irritated, itchy skin. Since fungal acne involves the hair follicles, that means you can get fungal acne anywhere on the body. It’s most common on the face, back and neck, but can present anywhere.
That’s why it’s important to understand what fungal acne looks like and how it develops. Read on to learn the symptoms and signs of fungal acne and what you can do to treat and prevent breakouts.
Because fungal acne can present like regular acne, it can be hard to distinguish which one you have. However, it’s extremely important to be able to tell the difference between comedonal acne vs fungal acne as fungal acne will not respond to typical acne treatments and needs special products. Traditional acne treatments can even make fungal acne worse, so it’s important to distinguish early on for best treatment.
Causes Of Fungal Acne
Wondering what causes folliculitis? There are many different causes of fungal acne, but in general, anything that allows the yeast to grow can contribute to outbreaks. Yeast like warm and moist environments, which is important to keep in mind when looking for causes of fungal acne so you can determine the proper cause and treatment.
- Weather – Fungal acne tends to be more prevalent in the summer months because of the heat, humidity and sweat
- Antibiotics – Antibiotics can kill the the good bacteria that make up our skin’s microbiome. When the microbiome becomes out of whack, it can lead to yeast and other bacteria to flourish, leading to folliculitis or fungal acne
- Tight clothes – tight clothing, especially clothing you have worked out in or sweat in can lead to fungal acne. The friction causes irritation and the damp environment is perfect for yeast to grow and grow
- Friction – anything that creates friction on the skin like scrubbing can lead to irritated skin and damaged hair follicles and make skin more susceptible to fungal acne
- Sweating – if you sweat a lot or workout, make sure you are showering as quickly as possible after you finish your workout or work. Keeping on damp, sweaty clothes creates a breeding ground for the yeast to flourish
Yeast grow in warm, moist environments. Fungal acne tends to flare in the summer months with heat, humidity and perspiration. It can also arise after treatment with medications such as antibiotics and steroids/prednisone. Many acne treatments are antibacterial, thus eliminating the normal skin bacteria and creating a perfect environment for yeast to proliferate and fungal acne to flare.
Symptoms Of Fungal Acne
One of the biggest reasons why fungal acne is so hard to get rid of is because it can look just like traditional acne. Most people have never even heard of fungal acne before and assume it’s just a breakout and treat it with traditional acne products, which can make it much worse.
- Clusters – fungal acne typically occurs in clusters where you’ll have a bunch of tiny spots in one small area. You may even have more than one cluster or several smaller clusters in one area
- Itching – fungal acne can also be itchy, so if you experience itchy skin all over or just in one area where there’s lots of acne-like spots, it could be an indication of fungal acne
- Size – malassezia folliculitis typically presents as smaller acne-like bumps or lesions and they’re usually all about the same size. Regular acne can vary in size and also present as larger pimples like cysts, whereas fungal acne will just be a lot of the same smaller pimples
- Location – fungal acne tends to occur in one area or even all over. You may experience a breakout on the chin or forehead but you can also experience fungal acne all over the face or even on the body
The biggest giveaway of fungal acne is that it’s itchy and doesn’t respond to traditional acne treatments.
Fungal Acne Treatment

One of the best treatments for fungal acne is anti-fungal products, whether OTC or prescription. It can also be helpful to make some lifestyle changes or get better hygiene habits to completely get rid of fungal acne outbreaks. Here are some products and tips on how to get rid of fungal acne.
Anti-Fungals
The quickest way to get rid of fungal acne is by using an anti-fungal product. The good news is that there are many over the counter anti-fungal products like creams and even shampoos you can use to treat folliculitis. For stubborn cases, prescription treatments may be needed. Topical and oral anti-fungal treatments can be used to clear up the skin.
Here are some over the counter fungal acne treatments worth trying.
Shampoo
Many dandruff shampoos contain pyrithione zinc or selenium sulfide, which both have anti-fungal properties. Although it is a shampoo, you can still safely use it on your face or body when treating fungal acne.
For best results, make sure you leave the shampoo on for 3-5 minutes to allow the active ingredients to work properly.
Selsun Blue Shampoo
Designed to treat dandruff and seborrheic dermatitis, Selsun Blue can also treat fungal acne because of its active ingredient pyrithione zinc. It can safely be used on the face or body to treat pityrosporum folliculitis. It does tend to be a little drying for the face, so be sure to use a good moisturizer to combat any irritation.
Nizoral Anti-Dandruff Shampoo
Another great option is Nizoral shampoo which is also designed to help with dandruff. This shampoo contains Ketoconazole which is an anti-fungal and can help kill malassezia yeast. It can also be used on the face or body to help treat folliculitis.
Cream
Lotromin Anti-Fungal
This anti-fungal cream contains Clotrimazole which is typically used to treat athletes foot. Although the yeast that causes fungal acne and athletes foot are different, they are very similar and these types of OTC fungal creams can help treat fungal acne at home. It’s best to apply 2x a day for a few weeks to see results.
Anti-fungal creams are often sold over the counter to treat athletes foot and ringworm, but the active ingredients are anti-fungals, so they can be helpful for treating folliculitis.
The most common anti-fungal cream is Lotromin, which contains clotrimazole, but there are a few others like ketoconazole or butenafine which both work equally well for treating folliculitis.
Zinc Soap
If you don’t like the idea of washing your face or body with shampoo, zinc soap will be right up your alley. Formulated for the face and body, they use pyrithione zinc to help treat folliculitis and other conditions like seborrheic dermatitis. They also usually have added ingredients like plant oils and oats to soothe and moisturize the skin. Since shampoo can be drying, these bar soaps are more dry/sensitive skin friendly.
Noble Formula 2% Pyrithione Zinc Soap
This bar soap is one of the most popular OTC treatments for fungal acne and is actually often recommended by dermatologists and Reddit boards. The Pyrithione Zinc kills the yeast associated with fungal acne. Try lathering it up and leaving it on the skin for 3-5 minutes for best results. It can also be used on the face or body.
Azelaic Acid
Azelaic acid has been shown to be a great treatment for fungal acne. One study found that topical azelaic acid help to treat and prevent lesions and also reduce inflammation and calm redness.
Related Post: Which Is Better Azelaic Acid Or Salicylic Acid?
Shower More Often
Keeping the skin clean is important, especially if you sweat a lot. Try to shower as quickly as possible. You can
Avoid Tight Clothing
Tight clothing can cause friction and irritation, which can lead to hair follicle damage and make you more prone to malassezia folliculitis. Keep in mind that workout clothing tends to be tight, and when you have been sweating, the combo creates a breeding ground for the yeast to grow.
Try to avoid wearing workout clothes unless at the gym and shower/change clothes as soon as you can after a workout.
Prescription Treatments
For stubborn cases, a visit to the dermatologist may be warranted. A doctor can assess your skin and take swap to confirm presence of yeast. There are many prescription treatments for fungal acne including powerful topicals and even oral anti-fungals that may be needed.
What Are Closed Comedones
Closed comedones, or comedonal acne, are a type of non-inflammatory acne. These are small bumps found on the surface of your skin that look like whiteheads, but unlike regular whiteheads, closed comedones do not have a pore. They are caused by plugs or clogs in hair follicles that block oil from getting out onto the skin.
Comedonal acne is classified as a mild and non-inflammatory type of acne.
Comedones can be classified as either open comedones or closed comedones. Open comedones, or blackheads, are so named because they exposed to the air and when the pore is exposed to oxygen, the dirt, oil, bacteria, etc will turn black (hence the name blackhead).
Closed comedones, also known as whiteheads, are small bumps on the skin’s surface with no opening to the pore. They have a layer of skin cells over them so they appear flesh-colored usually, but can also be red.
Although many people think whiteheads have a head that can be popped, whiteheads and closed comedones are actually the same thing and cannot be popped. Most pimples that have a head are considered papules or pustules.
Closed comedones often appear on the forehead and chin, but can occur anywhere on the face and can even occur on the neck, chest, back or other areas of the body.
Causes Of Closed Comedones
Like regular acne, closed comdeones are caused by a combination of factors: sebum, bacteria and dead skin cells that lead to clogged pores and eventually acne. The causes of fungal acne vs closed comedones are actually very different! Let’s take a look in detail at what causes acne and comedones.
Dead skin cells
Our skin cells naturally shed on their own, but when skin becomes dry or dehydrated, the skin cell cycle can be affected and skin cells cannot naturally shed themselves. Other factors can cause issues with the skin cell cycle as well. When skin cells are not shedding properly, this can lead to a buildup of them on the skin which can results in rough skin texture and lead to clogged pores.
Excess oil
Our skin naturally produces sebum, or oil, to help keep the skin moisturized and the skin barrier strong. While we do need some oil to keep our skin happy, sometimes our skin produces too much oil, which can be a bad thing. Oil can get trapped in our pores, and along with dead skin cells, can lead to acne.
Bacteria
We naturally have bacteria on our skin, which make up our skin’s microbiome which is essential to our skin’s health and our overall health. However, the skin’s microbiome can easily become disrupted, which can lead to bad bacteria flourishing and causing acne.
Symptoms Of Comedonal Acne
Because fungal acne and closed comedones can both appear as tiny bumps, it can be hard to figure out which one you have. If you’re wondering what does comedonal acne look like, here are some tips on identifying them.
- Location – while fungal acne tends to show up in clusters, comedones will occur all over and are generally spaced out more. You may also only get comedos on the cheeks, chin or forehead
- Size – Comedones can differ in sizes and can be so small they’re not even visible to the naked eye. If the spots on your skin seem to be all different sizes, it’s a good indication you have comedonal acne
- Blackheads – if you also have blackheads and clogged pores, it could be a sign your acne is comedonal as opposed to fungal. Those with closed comedones are also prone to open comedones like blackheads. However, you can still have fungal acne and blackheads
Closed Comedones Treatment

If you’re wondering how to get rid of closed comedones, look no further! The best treatment for closed comedones is exfoliation with chemical exfoliants or a gentle physical exfoliant but they can also respond to other treatments like antibiotics, benzoyl peroxide and using non-comedogenic products. Here are some of the best tips and best products for closed comedones.
Retinoids
If you struggle with comedones, a good retinol or retinoid will be your best bet. The biggest contributor to comedones is dead skin cells getting trapped in the pores and the best way to fix that is retinoids.
Retinoids, like retinol, retin-a or tretinoin speed up cell turnover to prevent dead skin from sticking around and clogging pores.
The Ordinary Granactive Retinoid 2% Emulsion
This Granactive Retinoid has all the powers of retinol without the irritation. Not only can it help treat and prevent comedonal acne, but it can also help smooth skin texture, fade pigmentation and reduce lines and wrinkles. Although retinoids tend to cause some initial irritation and dryness, granactive retinoids tend to have less side effects but are still powerful enough to unclog pores and prevent comedonal acne from forming.
Related Post: Retinol vs Granactive Retinoid
Differin Gel Adapalene 0.1%
Once prescription-only, Differin gives you all the powers of prescription acne treatment now at home. Adapalene is a retinoid that is stronger than other OTC retinol products, so you know you’ll get good results with this. It helps to unclog pores, prevent comedones and even skin tone and texture.
AHA/BHA
Other chemical exfoliants like glycolic acid, lactic acid, mandelic acid or salicylic acid can also be helpful in treating comedonal acne (and are usually more gentle on the skin than retinoids).
AHA’s like glycolic acid work the same ways as retinol – they speed up cell turnover to prevent those pesky skin cells from clogging your pores.
BHA’s, however, may be more beneficial for treating closed comedones because they are oil-soluble, which means they can cut through the oil on your skin and penetrate deeper into the pores to unclog pores and remove any gunk before it causes comedones. BHA’s can also kill acne-causing bacteria and reduce redness and inflammation.
Related Post: Salicylic Acid Vs Glycolic Acid: Which Is Best For You?
The Ordinary AHA 30% + BHA 2% Peeling Solution
This peeling solution combines AHA and BHA to resurface the skin, unclog pores, brighten skin tone, fight acne and reduce lines and wrinkles. It’s a powerful peel that can help get rid of even the most stubborn comedones.
Related Post: What Products To Use After The Ordinary Peeling Solution
Azelaic Acid
If you suffer from closed comdedones, azelaic acid is one of the best ingredients you can add into your skincare routine. Azelaic acid kill acne causing bacteria and helps calm down inflammation in the skin. It’s also a keratolytic agent which means it speeds up cell turnover and exfoliates away dead skin cells. It’s also been shown to be a comedolytic agent, which means that it prevents comedones from forming. While the treatment for fungal vs comedonal acne tends to be different, azelaic acid is one treatment that can treat both types.
The Ordinary Azelaic Acid Suspension 10%
With 10% Azelaic acid, this is a powerful OTC treatment that can help treat and prevent comedonal acne. It also helps to smooth skin texture, unclog pores and reduce redness. It’s incredibly affordable, but the texture tends to be a little gritty but it works very well.
Paula’s Choice 10% Azelaic Acid Booster
If you can’t get past the texture of The Ordinary’s Azelaic Acid, this serum is for you. It also contains 10% Azelaic Acid, along with salicylic acid to clarify and licorice to brighten the skin and fade hyperpigmentation.
Benzoyl Peroxide
Benzoyl peroxide is an antibacterial ingredient that can help treat acne, including closed comedones. Benzoyl peroxide works by killing the bad bacteria on your skin to reduce inflammation in the skin.
La Roche Posay Effaclar Duo Acne Treatment
This treatment combines 5.5% Benzoyl Peroxide to kill acne causing bacteria and LHA to help gently exfoliate the skin and unclog pores. While benzoyl peroxide tends to by drying, this formula uses microencapsulated BP to help reduce potential irritation and dryness. It also has glycerin to help rehydrate the skin and prevent flaking or dryness. It’s no wonder it’s one of the best La Roche Posay products.
Sulfur
Sulfur can also be beneficial in helping to treat open and closed comedones. Sulfur works by killing the acne-causing bacteria and also has antifungal, antibacterial, and keratolytic activity. The keratolytic activity can be extremely beneficial in treating closed comedones because it helps to break down dead skin cells.
Origins Out Of Trouble 10 Minute Mask
This clay mask is like an all over version of a drying lotion – with zinc, sulfur, camphor and clay, this is a powerful mask that can dry out pesky pimples, unclog pores and exfoliate the top layer of the skin for smoother, softer texture.
Kate Somerville EradiKate® Daily Cleanser Acne Treatment
This sulfur cleanser is designed for daily use to help clear skin by killing acne causing bacteria and breaking down dead skin cells to keep them from turning into comedones. Honey and oat extracts are also added to keep the skin hydrated since sulfur tends to be drying.
Non-Comedogenic Products
If you’re struggling with closed comedones, you’ll want to avoid products which contain comedogenic ingredients like mineral oil and coconut oil because these can clog your pores. You’ll want to choose products that are labeled “non-comedogenic” or “oil-free” so the product won’t clog your pores.
Fungal Acne Vs Closed Comedones Similarities & Differences
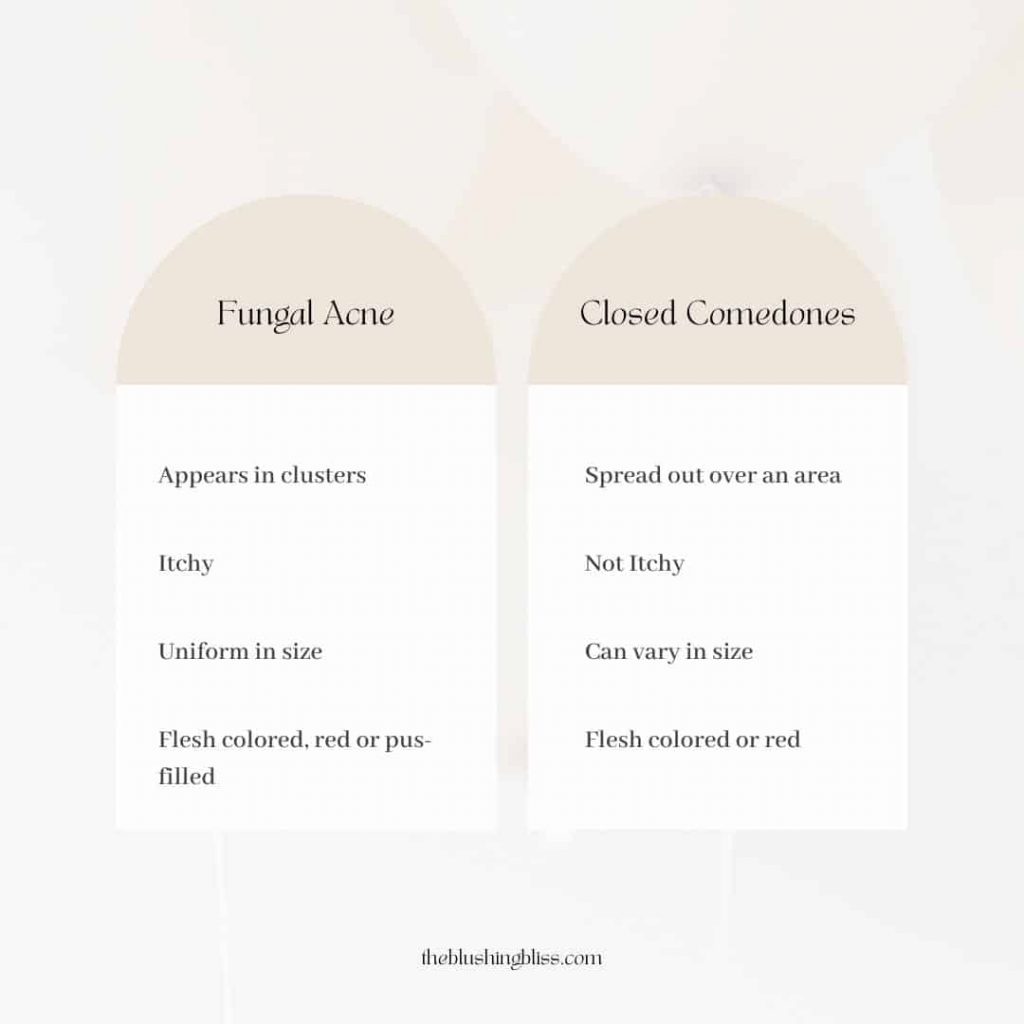
The major difference between the two is that fungal acne is caused by an overgrowth of Malassezia yeast, whereas closed comedones are caused by a combination of dead skin, bacteria, oil and dirt clogging pores.
Here’s a rundown of pityrosporum folliculitis fungal acne vs closed comedones to help understand the major differences between the two.
Since they’re caused by different things, treatment will be different depending on which one you have. And treatment for comedonal acne can actually make fungal acne flair up, so it’s important to distinguish early on for best treatment.
Fungal acne will require anti-fungals to kill the overgrowth of yeast.
Comedonal acne will need treatments that kill acne causing bacteria and treatments that speed up cell turnover to keep dead skin cells from clogging pores.
Fungal Acne
Comedonal Acne
How To Tell If You Have Closed Comedones Vs Fungal Acne
Distinguishing between closed comedones and fungal acne can be tricky, especially since they tend to look very similar. But with a few helpful tips, you can likely tell if you have fungal acne or comedonal acne. However, for the most accurate diagnosis, it’s best to see a dermatologist who can swab the skin and confirm the presence of Malassezia yeast.
- Is your skin itchy? If yes, this is a good indication that you have fungal acne
- Does your acne appear in clusters? Then there’s a good chance you’re suffering from fungal acne
- Are the bumps smaller and uniform in size? Another indication of fungal acne
- Do you also have blackheads and clogged pores? This could indicate that you have comedonal acne vs fungal
- Do the bumps appear spread out and all over (not clustered in areas)? If so, it’s most likely comedones
Keep in mind, this is a general guide and while it’s usually easy to distinguish between fungal vs comedonal acne, it can still be a little tricky. You can also have both comedonal and fungal acne which makes diagnosis and treatment more complicated.
What Causes Fungal Acne Vs Closed Comedones?
Fungal acne is caused by an infection in the hair follicle, usually because of an overgrowth of malassezia yeast. Closed comedones are caused from dead skin cells, dirt, bacteria and oil clogging the pores.
- Fungal Acne – caused by an overgrowth of yeast
- Closed Comedones – caused by a mixture of dead skin cells, dirt, bacteria and oil
Fungal Acne Vs Closed Comedones FAQ’s
Is comedonal acne the same as fungal acne?
No, fungal and comedonal acne are very different. Their causes, symptoms and treatment are all different. Comedonal acne is caused by a build up of dead skin, dirt, oil and bacteria in the pore, leading to a clogged pore and a flesh-colored bump.
Fungal acne is caused by an overgrowth of yeast that is commonly found on the skin. This leads to an infection in the hair follicle which presents as flesh color bumps that are often clustered and itchy.
Can I pop fungal acne?
Fungal acne can vary in presentation including pus filled bumps, closed skin-colored bumps and more. While the pus filled bumps can be popped, it must be done safely to avoid further infection of surrounding hair follicles and scarring. It’s best to leave the popping up to professionals.
Should you squeeze closed comedones?
You can squeeze closed comedones to extract them, and this is oftentimes done in dermatologist offices or during facials with an esthetician. As long as you are safely doing the extractions, there is no issue with squeezing them. But, if in doubt, leave it to the professionals.
Is Fungal Acne Always Itchy?
Fungal acne is almost always itchy, but there can be some rare cases where it’s not. Fungal acne, comedonal acne and inflammatory acne can also all appear at the same time, which can certainly complicate diagnosis.
Do I Have Fungal Acne Or Closed Comedones?
Many people are able to diagnosed themselves at home by looking at the location and size of the lesions and whether or not the skin is itchy. However, some cases can be complicated to diagnose and may need a dermatologist to swab the skin to determine the presence of fungus like malassezia yeast.
How To Tell The Difference Between Fungal Acne And Closed Comedones?
It can certainly be difficult to distinguish between fungal acne vs closed comedones, but there are a few tips that can help you determine which one you are suffering from.
Fungal acne will usually be itchy and appear in clusters with spots all the same size. Fungal acne can also produce skin colored or red lesions as well as pustules with a head or lesions that look pus-filled.
Comedonal acne will not be itchy and can vary in size and location, but will not have a head or pus visible. However, you can have comedonal acne and inflammatory acne like pustules or papules, which can make it hard to distinguish between regular acne vs fungal acne.
What Are The Triggers To Fungal Acne?
The most common fungal acne triggers are: antibiotics, tight clothing, wet clothing being left of the skin (like after a workout). Certain skincare products can also feed the yeast, so if you have a particularly stubborn case of fungal acne, you may need to use a fungal acne safe routine.
How Do You Know If Your Acne Is Fungal?
In some cases it can be hard to determine if you have comedonal acne vs fungal acne and you may need to see a dermatologist to get a swap and see if there’s a presence of yeast.
In most cases, if you skin is itchy and you have a lot of small flesh colored bumps in a cluster or you have acne that’s not responding to traditional treatments, it’s a good indication you have fungal acne.
Can Fungal Acne Look Like Closed Comedones?
Fungal acne can look very similar to comedones, which makes it hard to distinguish between malassezia folliculitis fungal acne vs closed comedones. To help determine which one you have, look at the size and location. Fungal acne tends to be all the same size and appear in clusters. Whereas comedonal acne will be varying sizes and appear more spread out over an area.
Fungal acne, on the other hand, happens due to an overgrowth of yeast (malassezia). Yeast is a natural part of your skin. However, if there’s an overgrowth in the hair follicles, you can get an acne like breakout.
How Long Does It Take To Get Rid Of Comedonal Acne?
Like regular acne, it can take upwards of 3-6 months to see significant improvements in comedones. Although you should start seeing results in 4-6 weeks, full results won’t come until much later. If you are using acne treatments and not seeing any improvement, you may need to switch up your treatments or see a dermatologist.
Fungal Acne Vs Closed Comedones: Wrap Up
When it comes to fungal acne vs regular acne, it’s not always clear which one you have. However, it’s very important to distinguish early on because regular acne treatments can oftentimes worsen fungal acne. Fungal acne tends to appear in clusters and tends to be pretty itchy. Comedonal acne, on the other hand, will generally be more spread out and uniform in size. Treatment can vary depending on which type you have, but azelaic acid is a great ingredient that can actually treat both fungal and comedonal acne. While malassezia folliculitis and comedonal acne can easily be treated at home, some cases need a dermatologist to help get the skin condition under control. In some cases you can have folliculitis and comedonal acne, which can complicate treatment. In general, both conditions are easily treated either at home or by a dermatologist.
- Fungal acne and comedonal acne have different causes, symptoms and presentations. Although they can look very similar upon inspection, with a few helpful tips you can easily distinguish between the two
- Fungal acne can present as red or flesh colored bumps and may even contain pus. They are generally all the same size and tend to appear in clusters. They also tend to be itchy
- Closed comedones are flesh colored bumps that do not have an opening or a head. They can vary in size and are generally spread out through the area (for example, all over the cheeks)
- Fungal acne is caused by an overgrowth of yeast called Malassezia yeast, which is naturally found on this skin. When overgrowth occurs, this leads to infection in the hair follicles which results in acne like bumps
- Closed comedones are caused by multiple factors – dead skin cells, dirt, oil and bacteria. These will end up clogging the pore and leading to skin-colored bumps.
- Treatment for closed comedones include keratolytics and exfoliating agents to keep dead skin cells from getting trapped in the pores, which prevents them from forming. Salicylic acid, glycolic acid and retinols are great options to speed up cell turnover. Additionally azelaic acid and sulfur are also great treatment options
- Treatment for fungal acne is very different than traditional types of acne, like comedones. Anti-fungal agents are standard and can include topical creams for ringworm or jock itch or shampoos for dandruff. These anti-fungals kill the yeast that causes fungal acne. Azelaic acid and zinc can also be used. Lifestyle changes may help reduce fungal acne as well, which includes always washing after sweating or the gym and avoiding tight clothing
Related To Fungal Acne Vs Closed Comedones
- Best Fungal Acne Safe Face Washes
- Does Hyaluronic Acid Help Treat Acne?
- Does Triamcinolone Acetonide Help Acne?




